The Key Differences Between Depression and Bipolar Disorder
 I was 14-years-old when things started to feel different, but I had no idea what was going on. All I knew was that I was sad all the time. I struggled to get out of bed. I didn’t want to go to school and would find every excuse not to. I went from being a straight-A student to nearly failing every class. Everything felt meaningless, I felt worthless and life didn’t feel worth living.
I was 14-years-old when things started to feel different, but I had no idea what was going on. All I knew was that I was sad all the time. I struggled to get out of bed. I didn’t want to go to school and would find every excuse not to. I went from being a straight-A student to nearly failing every class. Everything felt meaningless, I felt worthless and life didn’t feel worth living.
At the recommendation of my guidance counselor and teachers, I went to see a psychiatrist who diagnosed me with depression and anxiety. I had no idea what that meant, but he gave me a couple of prescriptions and told me I’d start to feel better.
Except I never did.
Thirteen years later, I walked into another psychiatrist’s office in a different state. He asked a ton of questions, and I answered honestly. At the end of that appointment, he diagnosed me with depression and anxiety, gave me a prescription for an antidepressant and told me in a few weeks, I’d feel better.
But once again, I never did. In fact, everything got so much worse to the point I was close to taking my own life.
At that point, my psychiatrist brought me in for an emergency appointment, and asked me the same questions he asked at our first appointment. I answered again – but this time, armed with more self-awareness and knowledge, I had different answers. This time, he diagnosed me with bipolar II disorder. He prescribed a common antipsychotic used to treat bipolar disorder and sent me on my way.
It’s been two-and-a-half years since that appointment, and while I still haven’t found the right medications to treat my bipolar disorder, I’ve learned a lot about mental illness in the process – especially around depression, bipolar disorder, and the similarities and differences between the two.
As it turns out, there are a lot of misconceptions around depression and bipolar disorder, mostly because they share many of the same symptoms. And just as I was misinformed – and misguided – for all those years, I’m sure there are many others out there going through the same thing. While I spend a lot of time on this blog sharing personal stories and messages of hope, I believe education is extremely important as well.
Today, I wanted to take some time to talk about depression, bipolar disorder, the symptoms of each and why bipolar disorder is commonly misdiagnosed as depression.
Table of Contents
3. When bipolar disorder is misdiagnosed as depression
4. Moving forward with your diagnosis

What is depression?
Depression, also known as major depressive disorder or clinical depression, is a common yet serious mental illness that negatively affects how you feel, the way you think and how you act.
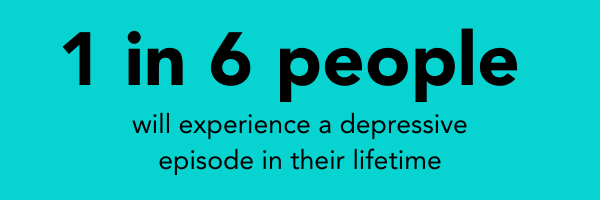
Depression is one of the most common mental illnesses and affects an estimated 1 in 15 adults in any given year. And 1 in 6 people will experience a depressive episode at some point in their life. It can strike at any time but typically first appears during the late teens to mid-20s.
Although women are more likely than men to experience depression, it’s important to note that depression doesn’t discriminate. People of all ages, races, genders, religions, lifestyles, and socioeconomic statuses are affected by depression (and mental illness as a whole).
How depression is different from being sad
There’s a general misunderstanding that depression is the same as being sad. But the reality is that it’s so much more than sadness.
Most people feel overwhelming sadness at some point in their life. The death of a loved one, loss of a job or the ending of a relationship are all difficult situations for a person to endure. And it’s normal for feelings of sadness or grief to follow.
But being sad is not the same as having depression. When those feelings of sadness turn into feeling helpless, worthless or useless; when they impact your day-to-day life; when they’re accompanied by suicidal thoughts or urges; or when those feelings last for many days, weeks or months – it could be something more than “just being sad.” These are often some of the first signs of depression.
Common symptoms of depression
The symptoms of depression can range from mild to severe and can include:
- Depressed mood, such as feeling sad, empty and hopeless
- Loss of interest or feeling no pleasure at all in most, if not all, activities
- Sudden weight loss or weight gain – or significant changes in appetite
- Sleeping too much or not at all (insomnia)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Decreased ability to think or concentrate
- Thoughts of harming yourself or others
A formal diagnosis must be made by a psychiatrist. And according to the DSM-5, a manual doctors use to diagnose mental disorders, you must experience at least five or more symptoms for at least two weeks.

What is bipolar disorder?
Bipolar disorder, formerly called manic depression, is a mental illness characterized by significant shifts in mood, energy, activity levels and the ability to carry out day-to-day-tasks. It causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
While depression and bipolar disorder share many similarities, there are a few key differences. The main distinguishing factor between depression and bipolar disorder is mania or hypomania. Whereas depression is unipolar – meaning it has no “up” period” – bipolar disorder has an “up” period, known as mania, along with depression.
Bipolar I disorder vs. bipolar II disorder
There are several types of bipolar disorder and related disorders. The two most common are:
- Bipolar I disorder
With bipolar I disorder, you’ve had at least one manic episode that was preceded or followed by a major depressive episode. In some cases, mania may trigger a break from reality (psychosis) and require hospitalization. - Bipolar II disorder
Bipolar II disorder is diagnosed after one or more major depressive episodes and at least one episode of hypomania. It’s also possible to have periods of level moods between episodes.
The highs in bipolar II disorder, called hypomania, are not as high as those in mania in bipolar I disorder. As a result, bipolar II disorder is sometimes misdiagnosed as depression because episodes of hypomania often go unnoticed (more on this in a bit).
Editor’s Note: Although bipolar II disorder is often seen as a milder form of bipolar I disorder, it is a completely separate diagnosis. While the manic episodes associated with bipolar I disorder can be severe and dangerous, people with bipolar II disorder tend to be depressed for longer periods of time, which can cause significant harm both mentally and physically.
Other related disorders include:
- Rapid cycling
Rapid cycling occurs when a person experiences four or more episodes of mania, hypomania or depression in a 12-month period. Rapid cycling can occur with any type of bipolar disorder. It’s often a temporary condition but can be longer-lasting for some people. - Mixed episodes
During a mixed episode, a person with bipolar disorder experiences both depression and mania or hypomania at the same time or in rapid sequence. One symptom – depression or mania/hypomania – may be more prevalent during the episode.
Mixed episodes have the potential to be dangerous because a person feels both extremely depressed and extremely euphoric at the same time – or within minutes or hours of each other. Therefore, someone experiencing a mixed episode is more likely to make impulsive or self-destructive decisions that could lead to harm against themselves or others. - Cyclothymic disorder
This is a milder form of bipolar disorder characterized by several episodes of hypomania and less severe depressive episodes that alternate for at least two years. - Not Otherwise Specified (NOS)
Bipolar disorder is classified as Not Otherwise Specified when it doesn’t follow a particular pattern. For example, a person may experience reoccurring hypomanic episodes without experiencing symptoms of depression. Or they may experience rapid swings between some symptoms of mania and some symptoms of depression.
Common symptoms of mania and hypomania
 While mania and hypomania are two distinct types of episodes, they share many of the same symptoms. Mania is often more severe and noticeable. In extreme cases, it may trigger a break from reality (psychosis) that requires hospitalization.
While mania and hypomania are two distinct types of episodes, they share many of the same symptoms. Mania is often more severe and noticeable. In extreme cases, it may trigger a break from reality (psychosis) that requires hospitalization.
On the other hand, a person experiencing a hypomanic episode may be able to carry on with their life normally. However, family and friends may notice changes in their mood or activity even if the person doesn’t see it themselves.
Personally, I’m very self-aware and often catch onto a hypomanic episode within a day or two. I can’t always hide my symptoms, but I work hard to make them less obvious to those around me.
Both manic and hypomanic episodes are characterized by at least three of the following symptoms:
- Having a higher, happier mood than normal **
- Increased irritability or rude behavior **
- Exaggerated sense of self-confidence or well-being (euphoria) **
- Decreased need for sleep (and feeling energized without it) **
- Higher activity or energy levels **
- Being much more social and talkative than usual
- Racing thoughts **
- Difficulty concentrating **
- Coming up with grand ideas or projects **
- Having a stronger desire for sex than usual
- Being more likely to engage in risky or impulsive behaviors like shopping sprees or spending large amounts of money**, sexual activities, using drugs or alcohol excessively or dangerous driving
** For education and transparency, these are hypomanic symptoms I typically experience. Not every symptom happens during every episode, and usually, one or two symptoms stand out as being the most extreme/noticeable.
Over the past two years, I’ve also had episodes that present more like manic episodes rather than hypomanic episodes, causing serious concern with my doctors (and myself). However, my diagnosis is still bipolar II disorder.

When bipolar disorder is misdiagnosed as depression
Because depression and bipolar II disorder, specifically, share many of the same symptoms – and because hypomania can be difficult to notice if you’re not specifically looking for it – it can lead to a misdiagnosis of depression.
A study published by Dr. Tanvir Singh and Dr. Muhammad Rajput found that 69% of people with bipolar disorder are initially misdiagnosed with depression. More than one-third of patients remain misdiagnosed for 10 years or more, although the average is around 5-7 years.
The highs in bipolar II disorder, known as hypomania, are not as high as those in bipolar I disorder (mania). As a result, the symptoms of hypomania often go unnoticed or unrecognized.
As someone living with bipolar II disorder, I can attest to the fact that sometimes, hypomanic symptoms are easily mistaken for “just feeling good” or “having a good day.” You’re happy, upbeat, more productive, more energized, and able to enjoy life. Hypomanic episodes aren’t always as obvious as little to no sleep, excessive irritability or making risky/impulsive decisions.
While being misdiagnosed for all those years was incredibly frustrating and led to a lot of mixed, mostly negative, feelings toward my doctors and even my family, I now understand how common it is and why the misdiagnosis happens so frequently.
Recognizing the symptoms of hypomania
I know firsthand how difficult it can be to notice the symptoms of hypomania – especially if you don’t fully understand bipolar disorder as a whole or even know that you have it.
 People misdiagnosed with depression often report that antidepressants make them feel worse than they did before, which was true in my case. Both times I was put on antidepressants, things slowly started to get worse.
People misdiagnosed with depression often report that antidepressants make them feel worse than they did before, which was true in my case. Both times I was put on antidepressants, things slowly started to get worse.
Both my doctors said it could get worse before it got better, but what I was experiencing didn’t seem normal. Something just didn’t feel right. Suddenly, nothing mattered, and I was constantly battling suicidal thoughts. Any day (or days) I missed my medication was significantly better than when I remembered it. Granted, those days were still tough – but they weren’t as bad.
As I later learned, taking antidepressants when you have bipolar disorder can actually make symptoms of bipolar depression worse or trigger a manic or hypomanic episode. That’s because depression and bipolar depression are not the same and therefore need to be treated differently.
Additionally, if something doesn’t feel right – whether it’s with your medication or general mood – pay close attention to your symptoms. If you have reoccurring depressive episodes that go away periodically and then return, here are some questions to ask yourself:
- Have I had periods lasting four or more days when my mood was especially energetic, high or irritable?
- Did I feel abnormally self-confident or social?
- Did I need less sleep than normal?
- Was I unusually talkative or hyper?
- Was I irritable or quick to anger?
- Did I think faster than usual (racing thoughts)?
- Was I easily distracted or having trouble concentrating?
- Was I coming up with grand ideas for new projects?
- Was I more goal-oriented or productive at work, school or home?
- Was I more involved in risky activities like excessive spending or sex with strangers?
- Did I feel – or did others notice – that I was doing or saying things that were unusual, abnormal or not like my usual self?
Ultimately, only your doctor, with your help, can determine whether you have depression or bipolar disorder. But as someone who didn’t know the signs – and was later in denial – I want to help others recognize the signs sooner so no one ever has to go through what I did for all those years.
Depression to bipolar disorder: When everything started to make sense
I was misdiagnosed with depression when I was 14. And it wasn’t until I saw a new doctor in Indiana when I was 27 that I was re-diagnosed with bipolar II disorder (only after he initially diagnosed me with depression).
I’ll be honest: It was really hard for me to come to terms with my new diagnosis of bipolar II disorder. I felt a wave of emotions in the days, weeks and even months after my diagnosis. Looking back, a lot of what I was experiencing was shame. There’s a huge stigma surrounding bipolar disorder, mostly because most people don’t understand it. And truthfully, even I didn’t fully understand it. Eventually, I found the silver lining in my new diagnosis.
Suddenly, so many experiences made sense. Like why the antidepressants I was prescribed didn’t work and why I felt better off of them. Granted, I was still depressed. But I felt significantly worse on antidepressants to the point where life never felt worth living.
And also the euphoric high I felt the day after I attempted suicide when I was 17. I remember sitting in my hospital bed, smiling, laughing, making jokes, saying everything was going to be fine. I wasn’t a danger to myself. It would never happen again.
Everyone – from my parents to the nurses and doctors – was frustrated with me and kept saying I didn’t understand the severity of my actions and that I wasn’t taking it seriously. I couldn’t explain why I had so much energy or why I felt like I could conquer the world and that everything would be just fine. But I did. To everyone else, I was making light out of a dark and serious situation that could’ve had severe long-term consequences.
But underneath all those layers and emotions was a 17-year-old girl experiencing the first hypomanic episode she could truly remember (although I believe there were several more before then). It was one of her more severe, noticeable episodes – and yet no one noticed.

Moving forward with your diagnosis...whatever it may be
Whether you’ve been diagnosed with depression or bipolar disorder, know that both illnesses are treatable with the right combination of medication, therapy and support. Hope and help are available. It’s not always an easy journey, and there will be times when you get frustrated or lose hope – especially if you’re misdiagnosed.
But I’ll tell you what I always tell myself:
You’re allowed to be angry. You’re allowed to hate the world and hate the process. You’re allowed to feel jealous when a close friend starts to feel better and you’re still struggling. You’re allowed to hate all the medications and visits to your psychiatrist. You’re allowed to have days when you hate therapy. You’re allowed to have days when you feel like you can’t do it anymore or days when you feel like it’s always going to be like this. You’re allowed to feel all the things you feel, and you need to know that all of those feelings are valid.
But the one thing you’re not allowed to do is give up. Not now. Not today. Not ever.
I know the pain feels permanent. I know it feels like it’s never going to get better. But I promise you: It won’t always be like this.
If you’ve lost hope and can’t fight for today, fight for better tomorrows. Know that tomorrow can be different – but the only way you’ll find out is if you keep fighting. Keep going. Keep surviving.

![The differences between depression and bipolar disorder [guide]](https://no-cache.hubspot.com/cta/default/5077772/9153543c-14de-4595-adee-3e8273a86eb6.png)
